gw insomnia . .
kadang ilang kadang g .
gw pernah g bisa tidur 5 hari,
dan hasilnya gw kek org bego dkampus,
bengong,
bego,
g connect . .
*************************************************************************************
ini artikel yg gw copas dr http://en.wikipedia.org/wiki/Insomnia#Types_of_insomnia
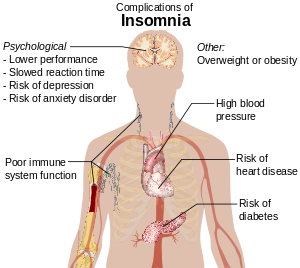
Insomnia is a symptom of any of several sleep disorders, characterized by persistent difficulty falling asleep or staying asleep despite the opportunity. Insomnia is a symptom, not a stand-alone diagnosis or a disease. By definition, insomnia is "difficulty initiating or maintaining sleep, or both" and it may be due to inadequate quality or quantity of sleep. It is typically followed by functional impairment while awake. Both organic and non-organic insomnia without other cause constitute a sleep disorder, primary insomnia.
Types of insomnia
Although there are several different degrees of insomnia, three types of insomnia have been clearly identified: transient, acute, and chronic.
- Transient insomnia lasts from days to weeks. It can be caused by another disorder, by changes in the sleep environment, by the timing of sleep, severe depression, or by stress. Its consequences - sleepiness and impaired psychomotor performance - are similar to those of sleep deprivation.
- Acute insomnia is the inability to consistently sleep well for a period of between three weeks to six months.
- Chronic insomnia lasts for years at a time. It can be caused by another disorder, or it can be a primary disorder. Its effects can vary according to its causes. They might include sleepiness, muscular fatigue, hallucinations, and/or mental fatigue; but people with chronic insomnia often show increased alertness. Some people that live with this disorder see things as though they were happening in slow motion, whereas moving objects seem to blend together. Can cause double vision.
Patterns of insomnia
The pattern of insomnia often is related to the etiology. Insomnia affects 1 in 3 people.
- Onset insomnia - difficulty falling asleep at the beginning of the night, often associated with anxiety disorders.
- Middle-of-the-Night Insomnia - Insomnia characterized by difficulty returning to sleep after awakening in the middle of the night or waking too early in the morning. Also referred to as nocturnal awakenings. Encompasses middle and terminal insomnia.
- Middle insomnia - waking during the middle of the night, difficulty maintaining sleep. Often associated with pain disorders or medical illness.
- Terminal (or late) insomnia - early morning waking. Often a characteristic of clinical depression.
Causes
Insomnia can be caused by:
- Psychoactive drugs or stimulants, including certain medications, herbs, caffeine, cocaine, ephedrine, amphetamines, methylphenidate, MDMA, methamphetamine and modafinil
- Fluoroquinolone antibiotic drugs, see Fluoroquinolone toxicity, associated with more severe and chronic types of insomnia
- Restless Legs Syndrome can cause insomnia due to the discomforting sensations felt and need to move the legs or other body parts to relieve these sensations. It is difficult if not impossible to fall asleep while moving.
- Any injury or condition that causes pain. Pain can preclude an individual from finding a comfortable position in which to fall asleep, and in addition can cause awakening if, during sleep, the person rolls over and puts pressure on the injured or painful area of the body.
- Hormone shifts such as those that precede menstruation and those during menopause
- Life problems like fear, stress, anxiety, emotional or mental tension, work problems, financial stress, unsatisfactory sex life
- Mental disorders such as bipolar disorder, clinical depression, generalized anxiety disorder, post traumatic stress disorder, schizophrenia, or obsessive compulsive disorder.
- Disturbances of the circadian rhythm, such as shift work and jet lag, can cause an inability to sleep at some times of the day and excessive sleepiness at other times of the day. Jet lag is seen in people who travel through multiple time zones, as the time relative to the rising and setting of the sun no longer coincides with the body's internal concept of it. The insomnia experienced by shift workers is also a circadian rhythm sleep disorder.
- Estrogen is considered to play a significant role in women’s mental health (including insomnia). A conceptual model of how estrogen affects mood was suggested by Douma et al. 2005 based on their extensive literature review relating activity of endogenous, bio-identical and synthetic estrogen with mood and well-being. They concluded the sudden estrogen withdrawal, fluctuating estrogen, and periods of sustained estrogen low levels correlated with significant mood lowering. Clinical recovery from depression postpartum, perimenopause, and postmenopause was shown to be effective after levels of estrogen were stabilized and/or restored.
- Certain neurological disorders, brain lesions, or a history of traumatic brain injury
- Medical conditions such as hyperthyroidism and rheumatoid arthritis
- Abuse of over-the counter or prescription sleep aids can produce rebound insomnia
- Poor sleep hygiene, e.g., noise
- Parasomnia, which includes a number of disruptive sleep events including nightmares, sleepwalking, violent behavior while sleeping, and REM behavior disorder, in which a person moves his/her physical body in response to events within his/her dreams
- A rare genetic condition can cause a prion-based, permanent and eventually fatal form of insomnia called fatal familial insomnia
- Parasites can cause intestinal disturbances while sleeping.[citation needed]
- Sometimes a rare case of insomnia is also seen in individuals who have long hours of consistent television watching or computer surfing.[citation needed]
Sleep studies using polysomnography have suggested that people who have insomnia with sleep disruption have elevated nighttime levels of circulating cortisol and adrenocorticotropic hormonepositron emission tomography (PET) scans indicate that people with insomnia have higher metabolic rates by night and by day. The question remains whether these changes are the causes or consequences of long-term insomnia. They also have an elevated metabolic rate, which does not occur in people who do not have insomnia but whose sleep is intentionally disrupted during a sleep study. Studies of brain metabolism using
Insomnia can be common after the loss of a loved one, even years or decades after the death, if they have not gone through the grieving process. Overall, symptoms and the degree of their severity affect each individual differently depending on their mental health, physical condition, and attitude or personality.
A common misperception is that the amount of sleep required decreases as a person ages. The ability to sleep for long periods, rather than the need for sleep, appears to be lost as people get older. Some elderly insomniacs toss and turn in bed and occasionally fall off the bed at night, diminishing the amount of sleep they receive.
Epidemiology
The National Sleep Foundation's 2002 Sleep in America poll showed that 58% of adults in the U.S. experienced symptoms of insomnia a few nights a week or more. Although insomnia was the most common sleep problem among about one half of older adults (48%), they were less likely to experience frequent symptoms of insomnia than their younger counterparts (45% vs. 62%), and their symptoms were more likely to be associated with medical conditions, according to the 2003 poll of adults between the ages of 55 and 84.
Diagnosis
Specialists in sleep medicine are qualified to diagnose the many different sleep disorders. Patients with various disorders including delayed sleep phase syndrome are often mis-diagnosed with insomnia.
If a patient has trouble getting to sleep, but has normal sleep pattern once asleep, a circadian rhythm disorder is a likely cause.
Sleep duration and mortality
A survey of 1.1 million residents in America conducted by the American Cancer Society found that those who reported sleeping about 7 hours per night had the lowest rates of mortality, whereas those who slept for fewer than 6 hours or more than 8 hours had higher mortality rates. Getting 8.5 or more hours of sleep per night increased the mortality rate by 15%. Severe insomnia - sleeping less than 3.5 hours in women and 4.5 hours in men - also led to a 15% increase in mortality. However, most of the increase in mortality from severe insomnia was discounted after controlling for comorbid disorders. After controlling for sleep duration and insomnia, use of sleeping pills was also found to be associated with an increased mortality rate.
The lowest mortality was seen in individuals who slept between six and a half and seven and a half hours per night. Even sleeping only 4.5 hours per night is associated with very little increase in mortality. Thus mild to moderate insomnia for most people may actually increase longevity and severe insomnia has only a very small effect on mortality.
As long as a patient refrains from using sleeping pills there is little to no increase in mortality associated with insomnia but there does appear to be an increase in longevity. This is reassuring for patients with insomnia in that despite the sometimes unpleasantness of insomnia, insomnia itself appears to be associated with increased longevity.
It is unclear why sleeping longer than 7.5 hours is associated with excess mortality.
Insomnia versus poor sleep quality
Poor sleep quality can occur as a result of sleep apnea or clinical depression. Poor sleep quality is caused by the individual not reaching stage 4 or delta sleep which has restorative properties. There are, however, people who are unable to achieve stage 4 sleep due to brain damage who lead perfectly normal lives.
Sleep apnea is a condition that occurs when a sleeping person's breathing is interrupted, thus interrupting the normal sleep cycle. With the obstructive form of the condition, some part of the sleeper's respiratory tract loses muscle tone and partially collapses. People with obstructive sleep apnea often do not remember awakening or having difficulty breathing, but they complain of excessive sleepiness during the day. Central sleep apnea interrupts the normal breathing stimulus of the central nervous system, and the individual must actually wake up to resume breathing. This form of apnea is often related to a cerebral vascular condition, congestive heart failure, and premature aging.
Major depression leads to alterations in the function of the hypothalamic-pituitary-adrenal axis, causing excessive release of cortisol which can lead to poor sleep quality.
Nocturnal polyuria, excessive nighttime urination, can be very disturbing to sleep.
Treatment for insomnia
In many cases, insomnia is caused by another disease, side effects from medications, or a psychological problem. It is important to identify or rule out medical and psychological before deciding on the treatment for the insomnia. Attention to sleep hygiene is an important first line treatment strategy and should be tried before any pharmacological approach is considered.
Non-pharmacological strategies
Non-pharmacological strategies are superior to hypnotic medication for insomnia because tolerance develops to the hypnotic effects as well as dependence can develop with rebound withdrawal effects developing upon discontinuation. Hypnotic medication is therefore only recommended for short term use. Non pharmacological strategies however, have long lasting improvements to insomnia and are recommended as a first line and long term strategy of managing insomnia. The strategies include attention to sleep hygiene, stimulus control, behavioral interventions, sleep-restriction therapy, patient education and relaxation therapy.
The latter can include meditation. For example Siddhārtha Gautama, 'The Buddha', recommended the practice of 'loving-kindness' meditation, or mettā bhāvanā as a way to produce relaxation and thereby, sound sleep.
A powerful non-pharmacological relaxation technique is floatation therapy which involves floating in a warmed salt solution in a float centre or personal float tank. The physiological relaxation effect is often effective in allowing natural sleep in the float tank and/or afterwards in bed rest. Those people who have experimented with floating as a treatment for insomnia, have sometimes found that one session is enough to initiate a normal sleep pattern.[citation needed]
Cognitive behavior therapy
A recent study found that cognitive behavior therapy is more effective than hypnotic medications in controlling insomnia.[citation needed] In this therapy, patients are taught improved sleep habits and relieved of counter-productive assumptions about sleep. Hypnotictolerance. The effects of cognitive behavior therapy have sustained and lasting effects on treating insomnia long after therapy has been discontinued. The addition of hypnotic medications with CBT adds no benefit in insomnia. The long lasting benefits of a course of CBT shows superiority over pharmacological hypnotic drugs. Even in the short term when compared to short term hypnotic medication such as zolpidem (Ambien), CBT still shows significant superiority. Thus CBT is recommended as a first line treatment for insomnia. medications are equally effective in the short term treatment of insomnia but their effects wear off over time due to
Medications
Many insomniacs rely on sleeping tablets and other sedatives to get rest. All sedative drugs have the potential of causing psychological dependence where the individual cannot psychologically accept that they can sleep without drugs[citation needed]. Certain classes of sedatives such as benzodiazepines and newer nonbenzodiazepine drugs can also cause physical dependence which manifests in withdrawal symptoms if the drug is not carefully titrated down. The benzodiazepinenonbenzodiazepine hypnotic medications also have a number of side effects such as day time fatigue, delayed reaction time, cognitive impairments and falls and fractures. Elderly people are more sensitive to these side effects. and
In comparing the options, a systematic review found that benzodiazepines and nonbenzodiazepines have similar efficacy which was not significantly more than for antidepressants.[25] Benzodiazepines did not have a significant tendency for more adverse drug reactions.[25] Chronic users of hypnotic medications for insomnia do not have better sleep than chronic insomniacs who do not take medications. In fact, chronic users of hypnotic medications actually have more regular nighttime awakenings than insomniacs who do not take hypnotic medications.[26] A further review of the literature regarding benzodiazepine hypnotic as well as the nonbenzodiazepines concluded that these drugs caused an unjustifiable risk to the individual and to public health and lack evidence of long term effectiveness. The risks include dependence, accidents and other adverse effects. Gradual discontinuation of hypnotics in long term users leads to improved health without worsening of sleep. Preferably hypnotics should be prescribed for only a few days at the lowest effective dose and avoided altogether wherever possible in the elderly.
Benzodiazepines
The most commonly used class of hypnotics prescribed for insomnia are the benzodiazepines. Benzodiazepines bind unselectively to the GABAA receptor. These include drugs such as temazepam, flunitrazepam, triazolam, flurazepam, midazolam, nitrazepam and quazepam. These drugs can lead to tolerance, physical dependence and the benzodiazepine withdrawal syndromeREM sleep. A further problem is with regular use of short acting sleep aids for insomnia, day time rebound anxiety can emerge. upon discontinuation, especially after consistent usage over long periods of time. Benzodiazepines while inducing unconsciousness, actually worsen sleep as they promote light sleep whilst decreasing time spent in deep sleep such as
Non-benzodiazepines
Nonbenzodiazepine sedative-hypnotic drugs, such as zolpidem, zaleplon, zopiclone and eszopiclone, are a newer classification of hypnotic medications. They work on the benzodiazepine site on the GABAA receptor complex similarly to the benzodiazepine class of drugs. Some but not all of the nonbenzodiazepines are selective for the α1 subunit on GABAA receptors which is responsible for inducing sleep and may therefore have a cleaner side effect profile than the older benzodiazepines. Zopiclone and eszopiclone like benzodiazepine drugs bind unselectively to α1, α2, α3 and α5 GABAA benzodiazepine receptors. Zolpidem is more selective and zaleplon is highly selective for the α1 subunit, thus giving them an advantage over benzodiazepines in terms of sleep architecture and a reduction in side effects. However, there are controversies over whether these non-benzodiazepine drugs are superior to benzodiazepines. These drugs appear to cause both psychological dependence and physical dependence though less than traditional benzodiazepines and can also cause the same memory and cognitive disturbances along with morning sedation.
Antidepressants
Some antidepressants such as amitriptyline, doxepin, mirtazapine, and trazodone can often have a very strong sedative effect, and are prescribed off label to treat insomnia.[33] The major drawback of these drugs is that they have antihistaminergic, anticholinergic and antiadrenergicsleep architecture. As with many benzodiazepines, the use of antidepressants in the treatment of insomnia can lead to physical dependence; withdrawal may induce rebound insomnia and actually further complicate matters in the long-term. properties which can lead to many side effects. Some also alter
Mirtazapine is known to decrease sleep latency, promoting sleep efficiency and increasing the total amount of sleeping time in patients suffering from both depression and insomnia [34] [35]
Melatonin and melatonin agonists
The hormone and supplement melatonin is effective in several types of insomnia. Melatonin has demonstrated effectiveness equivalent to the prescription sleeping tablet zopiclone in inducing sleep and regulating the sleep/waking cycle. One particular benefit of melatonin is that it can treat insomnia without altering the sleep pattern which is altered by many prescription sleeping tablets. Another benefit is it does not impair performance related skills.
Melatonin agonists, including ramelteon (Rozerem) and tasimelteon, seem to lack the potential for abuse and dependence. This class of drugs has a relatively mild side effect profile and lower likelihood of causing morning sedation. While these drugs show good effects for the treatment of insomnia due to jet lag, the results for other forms of insomnia are less promising.
Natural substances such as 5-HTP and L-Tryptophan have been said to fortify the serotonin-melatonin pathway and aid people with various sleep disorders including insomnia.
Antihistamines
The antihistamine diphenhydramine is widely used in nonprescription sleep aids such as Tylenol PM, with a 50 mg recommended dose mandated by the FDA. In the United Kingdom, Australia, New Zealand, South Africa, and other countries, a 25 mg to 50 mg recommended dose is permitted. While it is available over the counter, the effectiveness of these agents may decrease over time and the incidence of next-day sedation is higher than for most of the newer prescription drugs. Dependence does not seem to be an issue with this class of drugs.
Cyproheptadine is a useful alternative to benzodiazepine hypnotics in the treatment of insomnia. Cyproheptadine may be superior to benzodiazepines in the treatment of insomnia because cyproheptadine enhances sleep quality and quantity whereas benzodiazepines tend to decrease sleep quality.
Atypical antipsychotics
Low doses of certain atypical antipsychotics such as quetiapine, olanzapine and risperidone are also prescribed for their sedative effect but the danger of neurological and cognitive side effects make these drugs a poor choice to treat insomnia. Over time, quetiapine may lose its effectiveness as a sedative. The ability of quetiapine to produce sedation is determined by the dosage. Higher doses (300 mg - 900 mg) are usually taken for its use as an antipsychotic, while lower doses (25 mg - 200 mg) have a marked sedative effect, e.g. if a patient takes 300 mg, he/she will more likely benefit from the drug's antipsychotic effects, but if the dose is brought down to 100 mg, it will leave the patient feeling more sedated than at 300 mg, because it primarily works as a sedative at lower doses.
Eplivanserin is an investigational drug with a mechanism similar to these antipsychotics, but probably with less side effects.
*************************************************************************************
there you gooooooo, peeps !!
0 komentar to INSOMNIA raaawwrr !!:
Posting Komentar